Congenital diaphragmatic hernia (CDH) is a condition present at birth that affects how a baby’s lungs develop and function. It happens when there is an opening or weakness in the diaphragm, the muscle that helps with breathing. Because of this opening, organs from the abdomen (belly), such as the stomach or intestines, can move into the chest.
Congenital diaphragmatic hernia can be life-threatening, especially in newborns, because it interferes with normal breathing. Early diagnosis and proper treatment are extremely important for survival and long-term health.
What is a Congenital Diaphragmatic Hernia?
A congenital diaphragmatic hernia develops while the baby is growing in the womb. During early pregnancy, the diaphragm should fully form and separate the chest cavity (heart and lungs) from the abdominal cavity (stomach, liver, intestines).
The diaphragm (a dome-shaped muscle that helps us breathe) does not close completely in CDH. This allows abdominal organs to move upward into the chest, leaving less room for the lungs to grow.
This often causes lung hypoplasia (underdeveloped lungs), which is the main reason babies with CDH have breathing problems after birth.
Different Types of Congenital Diaphragmatic Hernia
There are several congenital diaphragmatic hernia types, depending on where the opening is located.
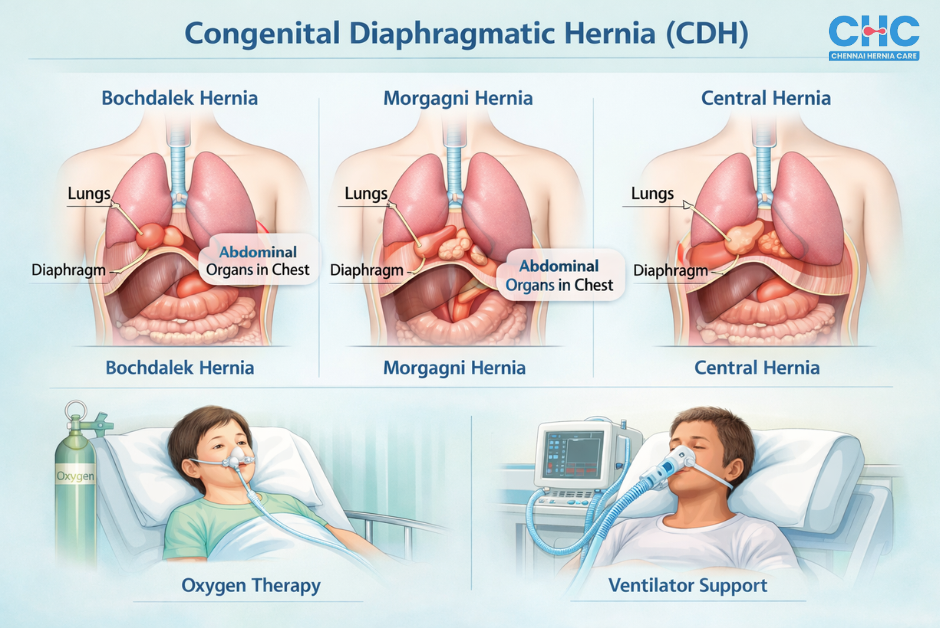
Bochdalek Hernia
The Bochdalek hernia is the most common type of CDH.
Key features:
- Occurs in the posterolateral diaphragm (back and side portion)
- Most commonly on the left side
- Allows organs like the stomach and intestines into the chest
This type usually causes severe breathing problems in newborns.
Morgagni Hernia
The Morgagni hernia is much rarer.
Key features:
- Occurs in the anterior diaphragm (front portion near the breastbone)
- Often affects the right side
- Symptoms may be mild or absent
This type may be discovered later in life, making it a form of diaphragmatic hernia in adults.
For a detailed comparison between Bochdalek and Morgagni hernias, please refer to our comprehensive medical insights on Bochdalek vs Morgagni Hernia.
Central Diaphragmatic Hernia
A central diaphragmatic hernia occurs due to weakness in the middle part of the diaphragm.
Important points:
- Rare
- Can affect both lungs
- Often causes serious breathing problems
Other Less Common Types of CDH
Other rare forms include:
- Eventration of the diaphragm (abnormally elevated diaphragm due to muscle weakness)
- Bilateral diaphragmatic hernia (defects on both sides)
These types often require specialised care.
Breathing Exercises: What Reddit Users Are Saying
In a Reddit discussion from the r/breathwork community, several medical insights were shared about managing congenital diaphragmatic hernia (CDH) through breathing exercises. While these insights come from personal experience, they align with several accepted medical practices for improving diaphragmatic function.
Key Medical Insights:
- Nasal Breathing: Breathing through the nose, especially during physical activity, helps protect the lungs and encourages optimal diaphragm use. It helps with regulating breathing and supports lung and heart function.
- Diaphragm Flexibility: Rather than strengthening the diaphragm, maintaining its flexibility is crucial. This flexibility comes from adequate CO2 levels and not over-breathing, which ensures the diaphragm can move effectively during both inhalation and exhalation.
- Pranayama Techniques: Specific techniques, such as gentle belly breathing, can help promote correct diaphragm motion, helping those with CDH develop better lung capacity over time. However, these exercises should be practised in moderation to avoid disrupting the body’s natural acid-base balance.
- Core Muscle Strengthening: Strengthening the transversus abdominis, the deepest core muscle, may help with breathing and diaphragm support. Gentle exercises such as planks or belly breathing with resistance (e.g., using a light book or brick) are suggested by some users as helpful.
Causes and Risk Factors for Congenital Diaphragmatic Hernia
Genetic Causes
Some congenital diaphragmatic hernia causes are linked to genetic or chromosomal conditions, such as:
- Trisomy 13
- Trisomy 18
These conditions affect normal organ development.
Environmental Factors
Possible contributing factors include:
- Smoking or alcohol use during pregnancy
- Exposure to certain medications
- Poor nutrition
Maternal Health Conditions
Maternal conditions that may increase risk include:
- Diabetes
- Obesity
- Advanced maternal age
In many cases, the exact cause remains unknown.
Symptoms of Congenital Diaphragmatic Hernia
Diaphragmatic Hernia in Newborns
Common symptoms include:
- Severe breathing difficulty
- Cyanosis (bluish skin due to low oxygen)
- Fast breathing
- One-sided chest movement
- Sunken abdomen
These symptoms usually appear soon after birth.
Diaphragmatic Hernia in Adults
When undiagnosed at birth, symptoms in adults may include:
- Shortness of breath
- Chest pain
- Digestive discomfort
- Recurrent lung infections
How is Congenital Diaphragmatic Hernia Diagnosed
Prenatal Diagnosis
CDH is often detected before birth using:
- Ultrasound (uses sound waves to create images)
- Fetal MRI (detailed imaging using magnets)
These tests help doctors plan specialised care.
Postnatal Diagnosis
After birth, diagnosis may include:
- Physical examination
- Chest X-ray
- CT scan or ultrasound
Diaphragmatic Hernia Radiology
Radiology (medical imaging) confirms the diagnosis, shows organ position, and helps guide surgical planning.
Treatment Options for Congenital Diaphragmatic Hernia
Surgical Treatment
Surgery is the primary treatment for CDH.
What surgery involves:
- Returning abdominal organs to the belly
- Closing the hole in the diaphragm
- Using a patch if the opening is large
Surgery is usually done once the baby is stable.
Post-Surgical Care
Babies may need:
- Ventilator support
- Oxygen therapy
- Treatment for pulmonary hypertension (high blood pressure in lung vessels)
- Nutritional support
Long-Term Outlook
Many children recover well but may need long-term follow-up.
Challenges in Treating Congenital Diaphragmatic Hernia
Possible complications include:
- Chronic lung disease
- Feeding difficulties
- Acid reflux
- Developmental delays
Prognosis and Quality of Life After Treatment
Outcomes for Children
Survival rates have improved significantly with modern care.
Long-Term Effects
Some children may experience:
- Reduced lung strength
- Frequent respiratory infections
- Learning difficulties
Early support improves quality of life.
Recent Advancements in Congenital Diaphragmatic Hernia Treatment
Recent advancements include:
- Minimally invasive surgery
- Improved ventilator support
- Fetal interventions (treatments before birth)
- Better prenatal risk assessment
Prevention and Future Directions
There is no guaranteed way to prevent CDH, but:
- Genetic counselling may help high-risk families
- Healthy pregnancy habits are encouraged
- Ongoing research continues to improve outcomes
Conclusion:
Congenital diaphragmatic hernia is a complex condition, but early diagnosis, proper imaging, timely surgery, and coordinated care significantly improve outcomes. Understanding the types, symptoms, causes, and treatment options helps families feel informed and supported.
With continued medical progress, children born with CDH have an increasingly hopeful future.
At Chennai Hernia Care, we offer comprehensive care and expert guidance for managing hernia conditions. Contact us today to schedule a consultation and receive personalised, high-quality care.
References: NIH Genetics | Children’s Hospital of Philadelphia | CDC | MedlinePlus | Radiopaedia | StatPearls | Children’s Hospital Colorado | Cleveland Clinic | NHS | Johns Hopkins Medicine | Radiopaedia
Our Medical Review Process:
Our content goes through a structured review process to ensure medical accuracy and reliability.
Written By: Editorial Team, Chennai Hernia Care
Reviewed By: Dr. Deepak Subramanian, MS, FMAS – Laparoscopic & Bariatric Surgeon
Last Updated: October 13, 2025